I am a person with no clinical or “care” background. But after almost forty years in senior management and executive roles across the spectrum of health and aged care – particularly aged care – I have gathered some insights into the nature of care being provided throughout our care services.
And before I suggest anything more, let me say this – my view is that if the major hospitals around Australia – public and private – were put under the same scrutiny and regulatory framework that residential aged care services are for the quality and accreditation of services that are provided in and through them, we would see hospitals falling into sanctions.
I am of the view that we have an aged care system that is too focused on beating the regulatory compliance framework as opposed to funding and providing appropriate levels of care and support to all clients.
On the one hand I am an incredibly strong advocate of high quality services accompanied with some form of accreditation. On the other hand, I believe we have an aged care accreditation system that we can really ill afford.
It underpins inadequate funding levels that cannot provide enough resources for many providers to meet the expressed needs of care for residents. In the same way, our community aged care system is creaking because we cannot provide enough funding for the community aged care packages assessed by the Australian Government as needed by our citizens.
I hear staff all over Australia clamouring, not always for more wages, but for more pairs of hands to do the work. To do more than the system underpins…To go the extra mile… To sit for a few minutes when that is what the client really wants, and really needs… To spend time hearing what the real story is…
To quote a UK study of its Home Help services from the early 1980s – “Too much Charring and not enough Chatting”.
I could ask the question – Which provides more care, the Chatting or the Charring? Neither is necessarily more correct, but often we cannot even get to the question. The bureaucratisation of aged care is with us and the paperwork must be done at our own peril.
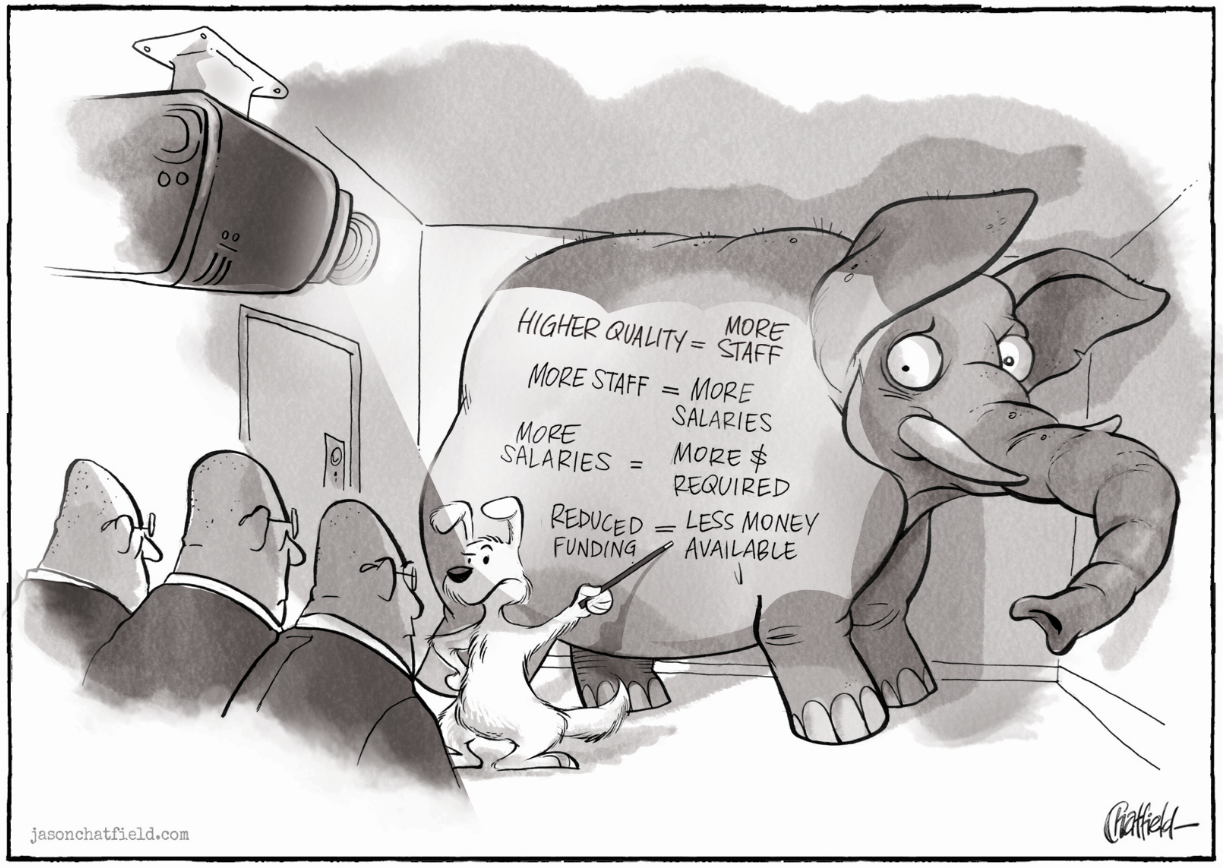
I have colleagues that will not (at this time) support minimum staff ratios. Quite rightly they see them as an un-affordable cost under the current funding methodology. How sad that we do not all see them as providing perhaps the single greatest opportunity right now to see a reduction in abuse, and a reduction in short cuts in care. How sad that we do not see minimum staff ratios as an opportunity to support our staff and see a visual improvement in the increased in quality of care. But implementation of minimum staff ratios will be quite costly.
I am still of the view that in Australia we have one the best aged care systems in the world. But for a range of reasons it is creaking.
Let’s all is to consider how much of a cost is there to stop, take stock, and with the next round of changes, really consider the long term impact of where we are heading and fight more intensely to protect the rights of those who are dependent upon us, the general public, for their livelihoods?
And who knows – the Royal Commission might investigate several inter services aspects around care of our elderly folks? One matter that I have discussed for the past decade is how much more proactive care we can provide in our aged care facilities, that might actually have a positive, beneficial impact on our national health and hospital care services.
In the past twenty years we have missed the opportunity to think outside the square with respect to fixing major State based hospitals. As a “cohort” of patients, frail elderly people are significant and frequent users of hospital services. Perhaps if we reviewed the aged care sector and its inherent possibilities we might find better solutions to our hospital problems.
Chatfield’s cartoon below was first published by me in December 2010 in an article containing many of the words in the commentary above. Not much has changed it seems!
To fix hospitals, first fix aged care!

I get it… Do You?